新冠带来又一挑战!下一步可能是“痴呆症浪潮”
生物探索
2022/08/12
论文一
论文标题:COVID-19 and olfactory dysfunction: a looming wave of dementia?
作者:Leslie M. Kay
期刊:Journal of Neurophysiology
发表时间:2022/07/27
数字识别码:10.1152/jn.00255.2022
摘要:Olfactory dysfunction is a hallmark symptom of COVID-19 disease resulting from the SARS-CoV-2 virus. The cause of the sudden and usually temporary anosmia that most people suffer from COVID-19 is likely entirely peripheral – inflammation and other damage caused by the virus in the sensory epithelium inside the upper recesses of the nasal cavity can damage or prevent chemicals from properly activating the olfactory sensory neurons. However, persistent olfactory dysfunction from COVID-19, in the form of hyposmia and parosmia (decreased or altered smell) may affect as many as 15 million people worldwide. This epidemic of olfactory dysfunction is thus a continuing public health concern. Mounting evidence suggests that the SARS-CoV-2 virus itself or inflammation from the immune response in the nasal sensory epithelium may invade the olfactory bulb, likely via non-neuronal transmission. COVID-19 related long term olfactory dysfunction and early damage to olfactory and limbic brain regions suggests a pattern of degeneration similar to that seen in early stages of Alzheimer's, Parkinson's and Lewy Body dementias. Thus, long term olfactory dysfunction coupled with cognitive and emotional disturbance from COVID-19 may be the first signs of delayed onset dementia from neurodegeneration. Few treatments are known to be effective to prevent further degeneration, but the first line of defense against degeneration may be olfactory and environmental enrichment. There is a pressing need for more research on treatments for olfactory dysfunction and longitudinal studies including cognitive and olfactory function from patients who have recovered from even mild COVID-19.
论文二:
论文标题:SARS-CoV-2 and the central nervous system: Emerging insights into hemorrhage-associated neurological consequences and therapeutic considerations
作者:Joy Mitra, Manohar Kodavati, Vincent E. Provasek, K.S. Rao, Sankar Mitra, Dale J. Hamilton, Philip J. Horner, Farhaan S. Vahidy, Gavin W. Britz, Thomas A. Kent, Muralidhar L. Hegde
收起
期刊:Ageing Research Reviews
发表时间:2022/07/16
数字识别码:10.1016/j.arr.2022.101687
摘要:
Coronavirus disease 2019 (COVID-19), caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) continues to impact our lives by causing widespread illness and death and poses a threat due to the possibility of emerging strains. SARS-CoV-2 targets angiotensin-converting enzyme 2 (ACE2) before entering vital organs of the body, including the brain. Studies have shown systemic inflammation, cellular senescence, and viral toxicity-mediated multi-organ failure occur during infectious periods. However, prognostic investigations suggest that both acute and long-term neurological complications, including predisposition to irreversible neurodegenerative diseases, can be a serious concern for COVID-19 survivors, especially the elderly population. As emerging studies reveal sites of SARS-CoV-2 infection in different parts of the brain, potential causes of chronic lesions including cerebral and deep-brain microbleeds and the likelihood of developing stroke-like pathologies increases, with critical long-term consequences, particularly for individuals with neuropathological and/or age-associated comorbid conditions. Our recent studies linking the blood degradation products to genome instability, leading to cellular senescence and ferroptosis, raise the possibility of similar neurovascular events as a result of SARS-CoV-2 infection. In this review, we discuss the neuropathological consequences of SARS-CoV-2 infection in COVID survivors, focusing on possible hemorrhagic damage in brain cells, its association to aging, and the future directions in developing mechanism-guided therapeutic strategies.
所属学科:
神经科学
生理学
生物
图片来源:Unsplash
导语:在感染新冠病毒之后,感染者的一大症状就是丧失嗅觉。既往研究指出,之所以新冠感染者会丧失嗅觉,是因为新冠病毒让嗅觉受体出现下调,使得人们无法正常检测到与气味有关的分子。而如今,根据相关报道,研究人员发现,与新冠感染相关的嗅觉丧失被认为是阿尔茨海默症的前兆。那新冠感染导致的嗅觉丧失,与人的认知能力之间究竟存在何种联系?
撰文|木子久
嗅觉功能障碍是新冠病毒的其中一项标志性症状,因新冠病毒而导致的持续性嗅觉功能障碍,以嗅觉减退和嗅觉异常(气味减少或改变)的形式影响全球多达1500万人。正因为如此,这种嗅觉功能障碍的流行是一个持续性的公共卫生问题。
越来越多的证据表明,新冠病毒本身或鼻感觉上皮中免疫反应引起的炎症可能会通过非神经元传播侵入嗅球。新冠感染相关的长期嗅觉功能障碍以及对嗅觉和边缘脑区的早期损伤表明了一种类似于阿尔茨海默病、帕金森和路易体痴呆早期阶段的退化模式。因此,新冠病毒引起的嗅觉功能障碍、认知和情绪障碍可能是神经退行性病变导致迟发性痴呆症的早期迹象。
新冠导致的嗅觉功能障碍,意味着“痴呆浪潮”即将到来?
近日,一项发表在Journal of Neurophysiology上,题为“COVID-19 and olfactory dysfunction: a looming wave of dementia?”的评论表示,新冠感染所导致的嗅觉丧失或许会增加感染者晚年患上痴呆症的风险,或会因此导致未来出现 “痴呆症浪潮”!
图1 评论截图(图源:[1])
嗅觉丧失是新冠病毒感染的标志性症状之一,约有77-85%的感染者因新冠病毒而出现嗅觉丧失或嗅觉异常,大部分人会很快恢复,但是会有一部分人经历持续性嗅觉丧失或嗅觉异常。既往有研究表明,新冠感染者的嗅觉上皮(位于鼻子上部,靠近嗅觉神经进入大脑嗅球的位置)中携带高病毒载量。
而嗅球是大脑中管理嗅觉并将感觉信息发送到大脑其他区域进行处理的结构,这些大脑区域与学习、记忆和情感有关,正如评论作者Leslie M.Kay博士所说:“所有这一切都意味着嗅球所关涉的远不止嗅觉,它还涉及记忆、环境、情感以及其他许多过程”。也正因为如此,新冠病毒影响的也不只嗅觉障碍,很有可能会影响人的相关认知功能,由于嗅觉上皮细胞靠近嗅球,即使在康复后,新冠感染也可能会影响认知功能。
阿根廷的研究人员与阿尔茨海默症协会联盟合作研究了新冠感染导致的慢性神经精神后遗症,他们对766名年龄在55岁至95岁的人群进行了一年的跟踪调查,对他们进行了一系列的身体、认知、神经、嗅觉等功能测试。研究人员发现,新冠导致的持续性嗅觉丧失是认知障碍的一个重要预测因素。
评论作者表示:“以前的流行病也支持这样的理论,即病毒入侵中枢神经系统可能是神经退行性病变的触发因素,导致神经功能受损。该审查提供的证据表明,通过新冠病毒感染和免疫反应引入嗅觉神经的炎症和对嗅球的损害也可能导致与嗅觉系统相关的大脑结构退化和认知障碍”。
大脑关键区域的新冠感染,或致大脑老化加速
新冠病毒感染对神经系统健康的影响越来越明显,休斯顿卫理公会的研究人员的一项最新研究发现,新冠病毒可使人们易患不可逆转的神经系统疾病,加速大脑老化,并增加中风和脑出血的风险。这项研究发表在Ageing Research Reviews上,题为“SARS-CoV-2 and the central nervous system: Emerging insights into hemorrhage-associated neurological consequences and therapeutic considerations”,研究表明,新冠感染会增加个体罹患神经系统疾病、中风、持续性脑损伤的几率。
图2 研究成果(图源:[2])
研究表明:
– 血脑屏障的主要成分、星形胶质细胞和脑微血管内皮细胞能够表达ACE2受体,其与SARS-CoV-2结合并紧密连接,导致神经炎症增加;
– 脉络丛细胞中的SARS-CoV-2感染可能影响人脑中的神经干细胞生态位,导致长期的神经病理学并发症;
– 新冠感染者死后,其大脑中活化的小胶质细胞和星形胶质细胞亚群类似于AD等神经退行性疾病的病理特征。
研究人员推测,新冠病毒感染可以刺激许多致病机制的激活,进而导致新冠感染者出现复杂形式的神经退行性疾病。
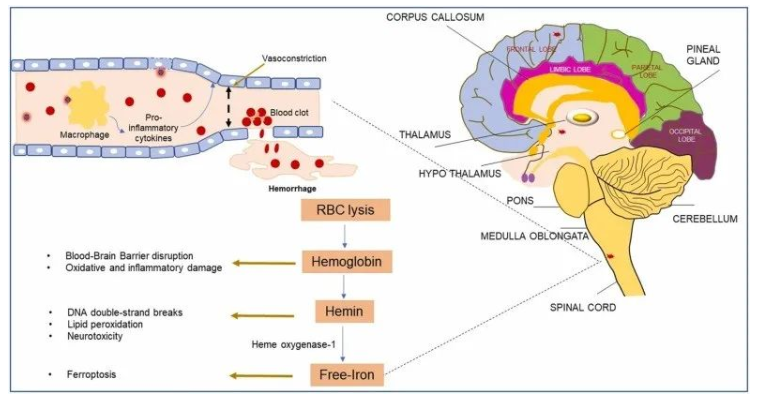
图3 新冠感染引起的大脑微出血及其潜在后果(图源:[2])
此外,研究还表明:
– 感染新冠病毒之后,感染者可能会出现慢性心血管异常,这或许是由于脑干和延髓区域的微出血相关神经元损伤而导致的;
– 凝血通路的过度激活导致15-30%对抗凝和抗预防治疗无反应的患者出现静脉血栓栓塞和血栓形成;
– 新冠感染可能导致涉及脑内皮细胞和微血管系统的CNS微血栓栓塞事件;
– 微出血是大脑衰老的预测因子,形成大量微出血可能表明新冠患者的大脑加速老化;
– 微出血在病理上与神经退行性病变、认知障碍和痴呆有关。
综上,研究表明,新冠感染引起的关键大脑区域微出血有可能加速感染者的大脑衰老,还可能导致复杂且不可逆转的神经退行性疾病,这是认知和运动功能的危险因素。
以上皆表明,感染新冠病毒对人体产生的影响还是比较大的,从嗅觉丧失、大脑微出血到神经退行性疾病,其所产生的每一个后果可能都会很严重。如今,新冠病毒又开始在我国部分地区肆虐起来,希望大家可以做好防护,保护好自己和家人。
参考资料:
[1]Kay LM. COVID-19 and olfactory dysfunction: a looming wave of dementia? J Neurophysiol. 2022 Jul 27. doi: 10.1152/jn.00255.2022. Epub ahead of print. PMID: 35894511.
[2]Mitra J, Kodavati M, Provasek VE, et al. SARS-CoV-2 and the central nervous system: Emerging insights into hemorrhage-associated neurological consequences and therapeutic considerations. Ageing Res Rev. 2022 Jul 16;80:101687. doi: 10.1016/j.arr.2022.101687. Epub ahead of print. PMID: 35843590; PMCID: PMC9288264.
本文引用自领:研究,点击原文:
关键词:新冠后遗症 长新冠 long covid



110X110.png)
110x110.png)